PATELLA STABILISATION SURGERY
Patella (kneecap) dislocations or instability are common. After a first-time dislocation the chances are that my expert advice and team working with a physiotherapist will rehabilitate the knee and you will return to full function.
However, there are times that the patella will dislocate again or even multiple times, and this may have been an issue since younger years.
In cases of ongoing patella instability you may have an abnormal positions of your patella. It may not be sitting within its groove (the trochlea) that makes it more prone to dislocation. This front part of your knee is called the patellofemoral joint. There are a number of features and positions that make the patella at risk of further dislocation that can be evaluated on x-ray and MRI:
- Rupture of the medial patellofemoral ligament (MPFL)
- A patella that sits higher up in its trochlea (patella alta)
- A tilted patella
- A trochlea groove that is shallow or has a bump (dysplasia)
- A quadriceps tendon pulling the patella in the wrong direction
The procedure that I perform to help with these issues are explained in detail below. The surgical plan is individualised to you and procedures are commonly combined to optimise outcome:
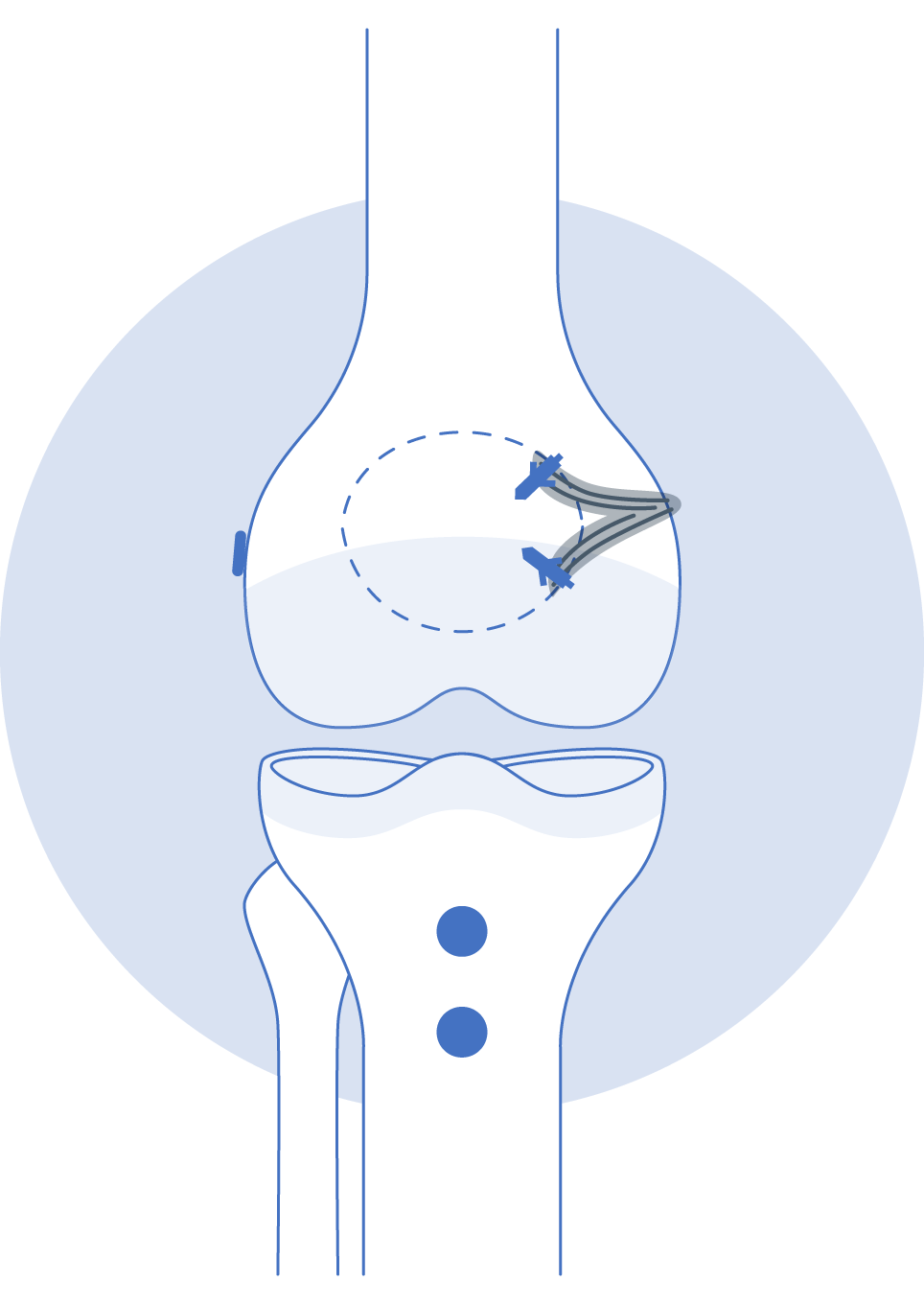
- Medial Patella-femoral Ligament (MPFL) Reconstruction; the ruptured ligament is reconstructed using a spare hamstring tendon from behind the knee
- Tibial Tubercle Osteotomy; changing the position of the bone insertion of the patella tendon. This has the effect of pulling the patella down and occasionally also inwards allowing it to sit perfectly in the trochlea grove
- Arthroscopy; key-hole access to the joint allowing assessment of patella tracking and treating any associated cartilage damage
Occasionally there is a significant issue with the development of the groove (trochlea) that the patella sits in. If I am concerned I will refer you on to a close specialist colleague that performs a rare procedure to help this:
- Trochleoplasty; a relatively rare and sub-specialist procedure to deepen the trochlea groove in cases when there is a bump seen